Shared investment
 Shared investment is a mechanism for joint ownership and responsibility, where all partners are ‘shareholders’. It needs cross-sectoral partnership at the highest level of decision making, as partners may need to reorient resources to meet mutually defined aims.
Shared investment is a mechanism for joint ownership and responsibility, where all partners are ‘shareholders’. It needs cross-sectoral partnership at the highest level of decision making, as partners may need to reorient resources to meet mutually defined aims.
A common language, goals, principles, strategies, measures of success and decision-making criteria are essential to guide investment and disinvestment. A partner may decide to disinvest where a funded program or service conflicts with the collectively agreed principles or priorities – for instance, duplication or poor return on investment.
Shared investment is a long-term proposition – it’s an iterative process with cycles of investment, evaluation and improvement.
Willingness to share decision making, including with community members, is paramount. For partners, shared investment requires ownership and accountability in proportion to their organisation’s budget and potential impact. For Healthy North Coast, the source of funding will be all commissioning funds (value: more than $23 million in 2018-19), which is the majority of their operating budget. Other partners may not have as much discretionary funding relative to their overall budget.
NCC approach to shared investment
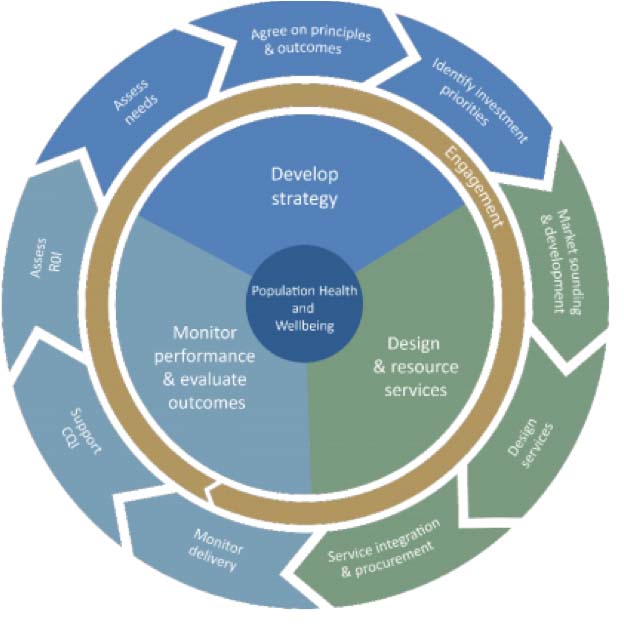
Shared investment differs from Healthy North Coast’s previous attempts to co-plan – shared investment is driven by implementation, with planning as only one stage of a clearly scoped joint process.
In 2018, the North Coast Collective published a concept paper for partners, Shared investment for population health on the North Coast (2.2MB pdf). The paper highlights escalating spending on health care and the potential to more efficiently target population health. It provides key foundations for shared investment including requirements, principles, business approaches and expected outcomes. A proposed approach is recommended along with next steps.
Why shared investment?
There are many reasons why we should be embracing shared investment. Total health care expenditure in Australia is rising faster than inflation and population growth. This has been fuelled by the growing prevalence of chronic disease and an ageing population, and is exacerbated by workforce challenges and an increasingly complex service sector.
Nearly three-quarters of total health expenditure is consumed by public and private hospitals (39%) and primary health care (35%) (AIHW 2018).
Siloed approaches to health funding create administrative ease but limited joint responsibility and action for population health outcomes. For example, the National Disability Insurance Scheme (NDIS) is a social insurance initiative jointly funded by the Australian, state and territory governments which provides essential services to eligible people with disabilities. The annual cost for the NDIS is about $14 billion though forecasts indicate significant year-on-year increases (Dickenson H 2018).
Research shows that healthcare is only a modest factor in preventing premature death. For example, in the USA the contribution of healthcare to preventing premature death is only 10% (New England Journal of Medicine 2007).
Healthcare reform agendas emphasise a whole-of-government approach to achieve improved population health. Applying resources from other sectors would have a substantial multiplying factor on Australia’s health investment (Bartlett C, Butler S and Haines L 2016).
References
AIHW, Australia’s Health 2018, Chapter 2.2: How much does Australia spend on health care? [online document].
Dickenson H (2018), Explainer: How much does the NDIS cost and where does this money come from? The Conversation website.
New England Journal of Medicine 2007, We can do better: Improving the Health of the American People, 357: 1221-1228.
Bartlett C, Butler S and Haines L, 2016, Reimagining health reform in Australia: Taking a systems approach to health and wellness, [online document], PricewaterhouseCoopers.
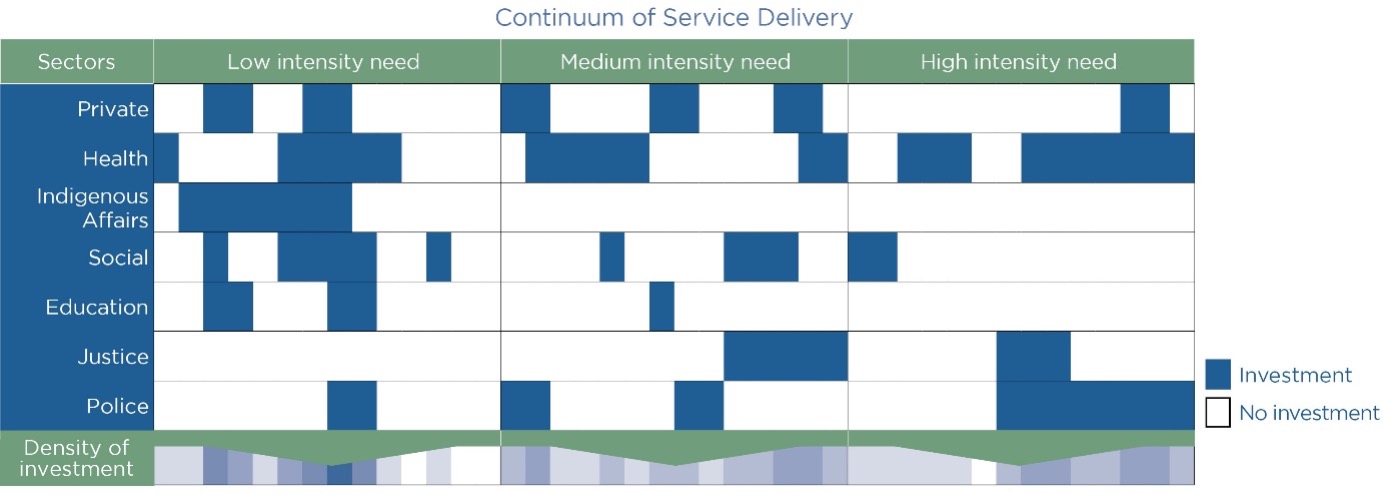
Cross-sectoral investment
This diagram shows the many sectors making significant contributions to health needs across the continuum of care. It indicates the probability of service duplication and service gaps when investment is considered collectively. Shared investment is a way to leverage cross sectoral action on shared health determinants and outcomes.